Pediatric diseases
- HOME
- Other than cancer(Whole Body, Others)
- Pediatric diseases
- Pediatric plastic surgery with excellent esthetics and functionality such as cleft lip and palate, microtia, macroglossia
Pediatric plastic surgery with excellent esthetics and functionality such as cleft lip and palate, microtia, macroglossia
24.04.03
This article was supervised by Dr. HIKOSAKA Makoto, Head, Division of Plastic Surgery, National Center for Child Health and Development(NCCHD)
Introduciton
The Division of Plastic Surgery at the National Center for Child Health and Development (NCCHD) delivers surgical treatment to help patients reintegrate into society by performing morphological and functional reconstruction of congenital and acquired defects. We aim to provide the most minimally invasive treatment, considering your child’s physical and psychological development and introducing the latest treatments. About 250 surgeries are performed under general anesthesia each year, 80% of which are for congenital anomalies, including about 50 cases/year related to cleft lip and palate, about 10-15 cases/year of plastic surgery (including bone lengthening, performed in collaboration with neurosurgery) for premature cranial suture fusion, about 10 cases/year of otoplasty of auricle formation for microtia, and a long history of treating macroglossia and other disorders.
Cleft lip and palate
Pursuing the best for patients through interdisciplinary medical care
EAJ: First, could you tell us about the treatment for cleft lip and palate, which is the most frequently treated condition?
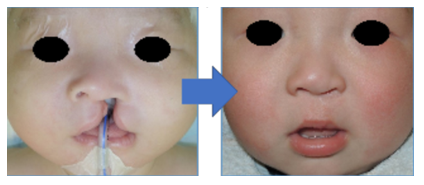
Dr. HIKOSAKA: Cleft lip and palate is a congenital condition in which clefts occur in the lips, palate (roof of the mouth), and upper jaw (gums) due to tissue defects or malunion during the embryonic period. There are various types of the disease, including cleft lip only, cleft palate only, and cheilognathopalatoschisis (cleft lip and cleft jaw).
The treatment policy for cleft lip and palate differs depending on the facility, but at NCCHD, our policy is to treat cleft lip, cleft palate, and cleft jaw in three stages. The first surgery is usually performed between 4 and 6 months of age.
As for symptoms, in many cases of cleft lip, the facial deformity is not limited to the lips but also extends to the nose, causing problems with cosmetics (appearance) as well as eating and speech difficulties. Cleft palate causes eating and speech problems because food and speech sound escape through the nose. In addition, the child may be prone to otitis media, may not have adequate midface development (“growth of the central part of the human face,” meaning the growth and development of the upper jaw, nose, and cheeks), and, in the case of cleft jaw, may have crooked dental problems due to teeth not growing in the cleft of the gums. NCCHD provides interdisciplinary medical care from pre-operative to post-operative care in collaboration with related medical departments such as plastic surgery, pediatrics, otorhinolaryngology, and dentistry. We also provide support to improve resilience (mental strength) so that children can lead a smooth social life after surgery.
Treatment period (for cleft lip and palate)
Dr. HIKOSAKA: After receiving the medical information, we will conduct an online medical consultation for about an hour in advance. Once a patient arrives in Japan, the hospitalization period will be approximately 10 days (3 to 4 days if the patient is only undergoing tests without surgery). We will see the patient once within a month after a patient is discharged from the hospital. After that, we generally continue to see the patient once a month for about six months, but we believe the schedule will be flexible depending on the patient’s situation, such as having them seen every three months or providing online consultations.
Velopharyngeal insufficiency
Conventional surgery? Autologous fat injection? The check on the applicability of each option is important
EAJ: After cleft lip and palate surgery, or due to post-operative growth, some patients come to the hospital complaining about speech sound escaping out of their nose (one of the symptoms of velopharyngeal insufficiency).
Dr. HIKOSAKA: Approximately 90% of children after surgery will acquire velopharyngeal closure function (palatal function in speech; closure function) to the extent that there are no problems in daily life. However, as the nasopharynx expands with growth, it is known that some patients lose the closing function gradually.
In the past, relatively major surgery was the only way to improve the closure function, so if the symptoms were mild, even if there were some inconveniences such as slurred speech, the patient was observed if it was judged that the surgery was not worth it. In recent years, however, a relatively low-impact treatment called autologous fat injection has become available, in which fat is suctioned from the thigh or other parts of the body using a thin cannula and injected into the posterior wall of the nasopharynx and submucosa of the soft palate to narrow the nasopharynx and improve its function.
Therefore, when a patient with symptoms of nasopharyngeal obstruction comes to our clinic, we will check on the applicability of each option as to whether a conventional, relatively large surgery such as pharyngoplasty or autologous fat injection is more suitable to balance the burden and effectiveness. The examination takes a full day, and along with a nasopharyngeal fiberscope, a speech-language pathologist will also will participate in diagnosis. Depending on the results, we will recommend either pharyngeal flap surgery or autologous fat injection. After the examination, treatment can be started directly, or a patient can return to the home country to deliberate on the matter at home. It is around 5 to 6 years old that a speech-language therapist can assess closed function, and even if it is determined that there is no problem at that time, the function may decline around 15 to 6 years old, when the child grows taller. Patients may also come to the hospital because they are concerned about job opportunities or other opportunities. There are no restrictions on when autologous fat injection can be applied. Treatment is available as soon as you become aware of your child’s symptoms.
Microtia
Visits from overseas seeking high level of skill
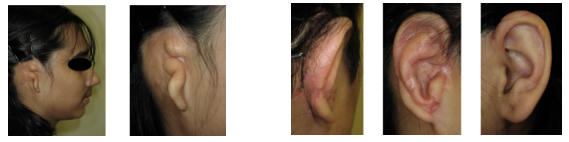
EAJ: I understand that you perform otoplasty with a high level of skill on patients with microtia who are born with small or defective auricles, and that patients from overseas sometimes come to you for treatment. What kind of treatment do you provide?
Dr. HIKOSAKA: Basically, plastic surgery is performed using the patient’s own costal cartilage. Treatment varies depending on the symptoms. In the first stage, a tissue expander (balloon-shaped silicone) is inserted and the skin is expanded over a period of about four months. In the second stage, rib cartilage is transplanted, and the patient is monitored over a period of about six months to ensure that the transplanted cartilage blends with the ear. Furthermore, in the third stage, auricular elevation and ear lobe formation are performed.
EAJ: Is there an appropriate time for treatment?
Dr. HIKOSAKA: Since the ear is said to reach 95% of its adult size at age 9, it can be used for life if it is formed around age 9 to be as large as the opposite ear (the one without the microtia). Costal cartilage is used to form the ears. After the age of 20, the cartilage becomes ossified and hardens, making surgery difficult. Therefore, we believe that treatment is recommended until the age of 17.
Macroglossia
Developing an original surgical technique that balances cosmetic and functional aspects
EAJ: I hear that you use a highly functional surgical method for macroglossia surgery.
Dr. HIKOSAKA: Macroglossia is a condition in which the tongue protrudes outside the lips when at rest, and symptoms include breathing, eating, speech, occlusion, and cosmetics. There are various methods for glossoplasty, but at NCCHD we perform an original surgical method called cruciate resection. It is technically more difficult than the conventional method of removing only the tip of the tongue because it is more complex, but its main feature is that it can ensure a higher level of function during speech while considering the child’s cosmetic features (sufficient reduction in size and thickness).
Message to patients
EAJ: Lastly, please give a message to patients and their families.
Dr. HIKOSAKA: Many diseases in the field of plastic surgery require long-term aftercare as the patient grows even after surgery. NCCHD is a general pediatric hospital that not only has an ICU, but also provides comprehensive interdisciplinary care on a daily basis. In addition to providing detailed medical care before and after surgery, we also provide care for both the child and the parents after the child is discharged from the hospital, starting around the age of 3, to support the child and their parents so that they can proactively engage in treatment and post-treatment life. All of our staff members are working meticulously to support your child’s growth as much as possible, so we appreciate everyone’s continued support.